Navigating the impact of freeze-thaw cycles on sperm can be daunting for couples pursuing IUI. Post thaw motility sperm is crucial, and here, we unpack the challenges it presents and reveal strategies to optimize motility for fertility success.
Key Takeaways
- Successfully freezing and thawing sperm is essential for IUI fertility treatments, with a post-wash TMSC greater than 10 million increasing the odds of pregnancy.
- The cryopreservation process, which protects and stores sperm at -196 degrees C using cryoprotectants, directly impacts post-thaw sperm motility and thereby influences IUI success rates.
- Improving post-thaw motility can be achieved through specific cryopreservation techniques, lifestyle adjustments, and supplements to enhance sperm quality, with IVF and ICSI as alternatives when motility remains low.
Understanding Post-Thaw Motility Sperm

In order to achieve a successful IUI, at least 5 million motile sperm must be present in the sample post-washing. If these numbers decrease after being frozen and thawed, fertility drugs may need to be taken into consideration for better results. For this procedure to have good prospects of success, it is ideal that a total motile sperm count exceeds 10 million. High levels of sperm movement following cryopreservation are also essential so fertilization can occur properly once placed inside the uterine cavity during ovulation time frame.
The Cryopreservation Process
To ensure successful fertility treatments, cryopreservation is a vital component. This process freezes and stores the biological sample in extreme cold conditions for later use. It can detrimentally affect sperm motility as evidenced by an IUI or artificial insemination procedure following examination of the cells through a sperm test. To complete this step, firstly one must collect semen then blend with protective substances to prevent damage during storage before freezing in specific thermally insulated containers which should remain at minus 196 degrees centigrade allowing them to remain viable for future utilization.
Factors Affecting Post-Thaw Motility
The motility of sperm can be lowered up to 50% during the freeze-thaw cycle, but preselection freezing has been found to increase rates. When it comes to fertility issues such as polycystic ovarian syndrome and unexplained infertility, quality is key. When cells are subjected to extreme temperatures like during a thawing process, they may suffer damage which affects their ability for capacitation and impede DNA integrity, all these damaging factors together reduce the probability that these cells will successfully fertilize an egg. A successful result requires optimal semen preservation techniques from beginning till end of each reproductive cycle.
Impact of Post-Thaw Motility on IUI Success Rates
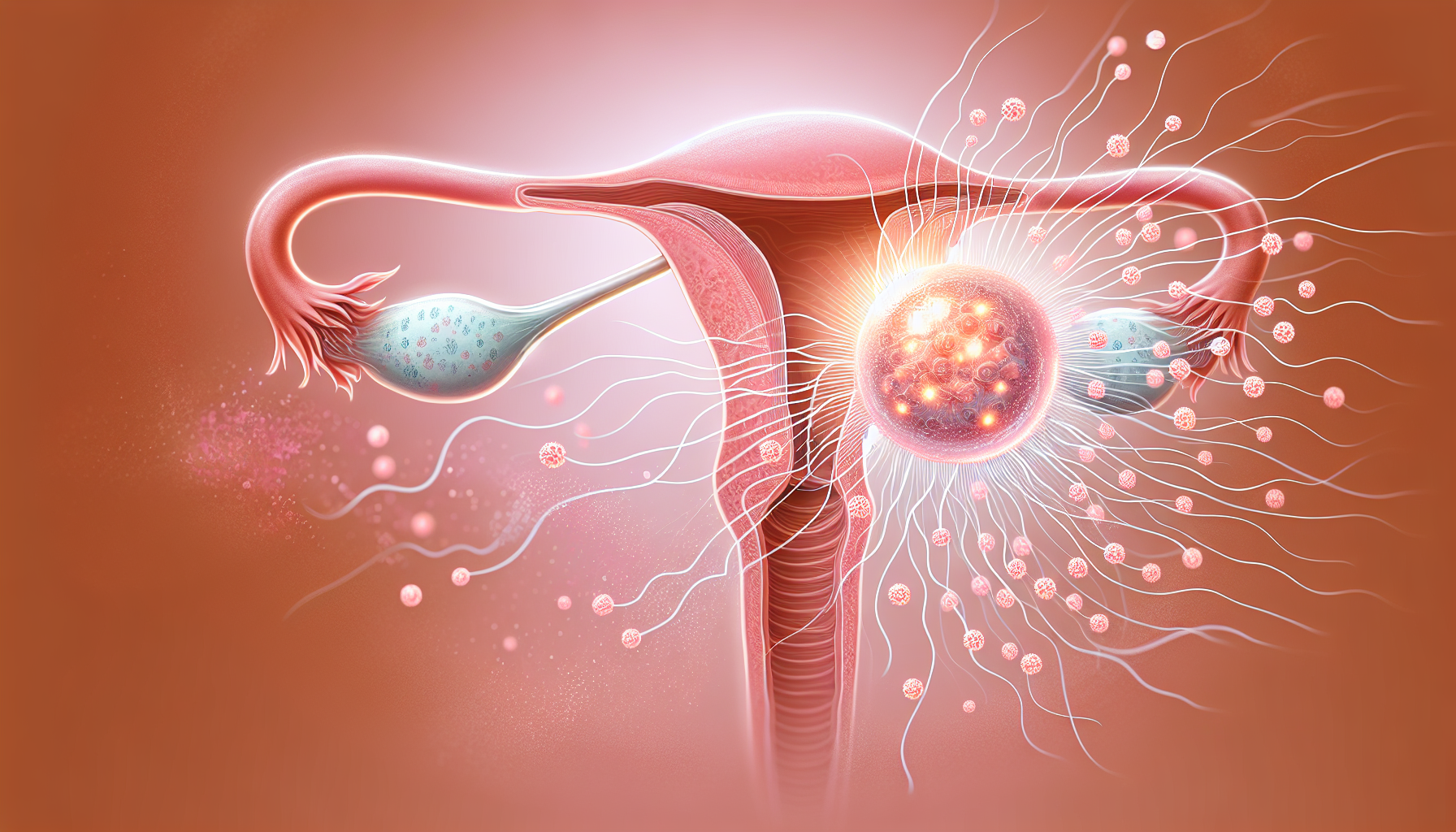
The correlation between high post-thaw motility, in particular the Total Motile Sperm Count (TMSC) and success rates of IUI is highly significant. The optimal level for TMSC appears to be more than 9 million. A fertility seesaw effect was observed with decreasing pregnancy rates as TMSC levels dropped below this point. Consequently, it stands that higher sperm counts have greater potential when seeking positive results through IUI treatments due to their influence on both pregnancy and success outcomes.
Donor Sperm vs. Partner Sperm
When it comes to the success of intrauterine insemination (IUI) procedures, there is no significant difference between donor sperm and partner sperm. Even more surprising, post-thaw motility rates are also similar for both sources of semen. This means that when considering fertility via IUI or any other method involving insemination with a sperm sample (be it from a partner or an anonymous donor), chances of pregnancy don’t necessarily depend on where the specimen originated, but rather how successfully those individual cells work towards fertilizing an egg.
Strategies to Improve Post-Thaw Motility

Selecting the right cryoprotectants for sperm and optimizing freezing techniques are two factors that may improve post-thaw motility. This selection can have an effect on the motility, viability and fertility of these cells when they thaw out again afterwards. Besides this technical aspect, lifestyle changes or taking specific supplements might also help with improving semen quality after being frozen. Both chemical properties as well as other aspects must be considered if better results in terms of mobility are to be expected.
Choosing the Right Cryoprotectant
When looking for a cryoprotectant to use in sperm freezing, much like the selection of an ideal shield for battle by a knight, one should consider its capacity for long-term storage and the effect on quality after thawing. Glycerol is often used along with sucrose or other sugars, but no single agent has been proven more successful than others at preserving high-level fertility. Keeping into account ice formation resistance as well as viability and specific procedures needed when working with this material will lead to better results too. Thus all these factors must be taken into consideration prior to selecting the right cryprotectant option appropriate for achieving desired outcomes linked to fertility preservation via semen cold storing techniques.
Optimal Freezing and Thawing Techniques
When processing sperm samples, the effectiveness of freezing and thawing techniques has a large influence on their motility. The use of cryoprotectants is crucial to protect the cells during this process and ice formation should be monitored properly in order to avoid damage. Maintaining viable storage conditions are also important for preservation so that osmotic stress can be reduced as much as possible.
The optimal temperature at which these sperm specimens should ideally be frozen lies between -196°C, with programmable slow-freezing or liquid nitrogen vapor being popular methods used for efficient thawing purposes afterwards. It’s imperative that once cooled down again they remain healthy enough when tested. Only then will fertility chances stay high upon future usage if needed accordingly.
Lifestyle Changes and Supplements
Making positive lifestyle adjustments can be very useful in increasing the quality of sperm. To this end, here are a few key suggestions: regulate weight, reduce alcohol consumption, stop smoking and steer clear from harmful substances. As well as find ways to manage stress levels effectively. By making these changes, it is possible to improve the health of your sperm – which could potentially result in improved post-thaw motility rates too.
To improve one’s way of living, certain supplements may also help support good semen performance. Such nutritional additives supply essential minerals and vitamins that could enhance characteristics like density, activity level (motility), shape (morphology) among others – all positives for better post-thaw mobility outcomes with regards to sperms’ viability/fecundity capabilities!
Monitoring Post-Thaw Motility: Semen Analysis and Quality Control

Semen analysis is an important quality control measure when it comes to monitoring post-thaw motility, which can drastically influence successful IUI outcomes. It involves evaluating various parameters such as sperm concentration, total motile count and morphology in order to understand the fertilizing potential of the semen sample. If necessary, Clomiphene citrate may be prescribed for improving fertility chances with IUI procedures. Keeping a watch on these components will ultimately ensure that high rates of success are achieved from intrauterine insemination (IUI).
Interpreting Semen Analysis Results
Semen analysis is not as complicated to interpret once you understand the basics. The results provide important information about sperm concentration, total motile count, and morphology. Motility plays a significant role in successful IUI since it shows how many are actively moving – more than 32% must be motile for an optimal result with 5 million or higher needed after processing of the sample. To ensure fertility success during IUI, there needs to be 40% overall movement or greater from these samemotile spermsamples which can then proceed into fertilization being made possible through them successfully reaching their goal destination!
Ensuring Quality Control in the Laboratory
In a fertility lab, quality control acts as the guard rails on a highway that guarantee an efficient and secure operation. Such measures involve examining supplies, monitoring equipment and executing daily tasks in order to ensure accurate outcomes with optimal semen analysis. Specifically, using swim-up before freezing alongside CryoSeeds and DTT can significantly boost post-thaw sperm motility. Technicians play an essential role in keeping up such standards so that when it comes to cryopreservation of sperm samples a high standard is maintained throughout the process. For this purpose, different pieces of equipment including floor protection mats, serum preparation machinery, and cryopreservation apparatus are used.
When to Consider Alternative Fertility Treatments
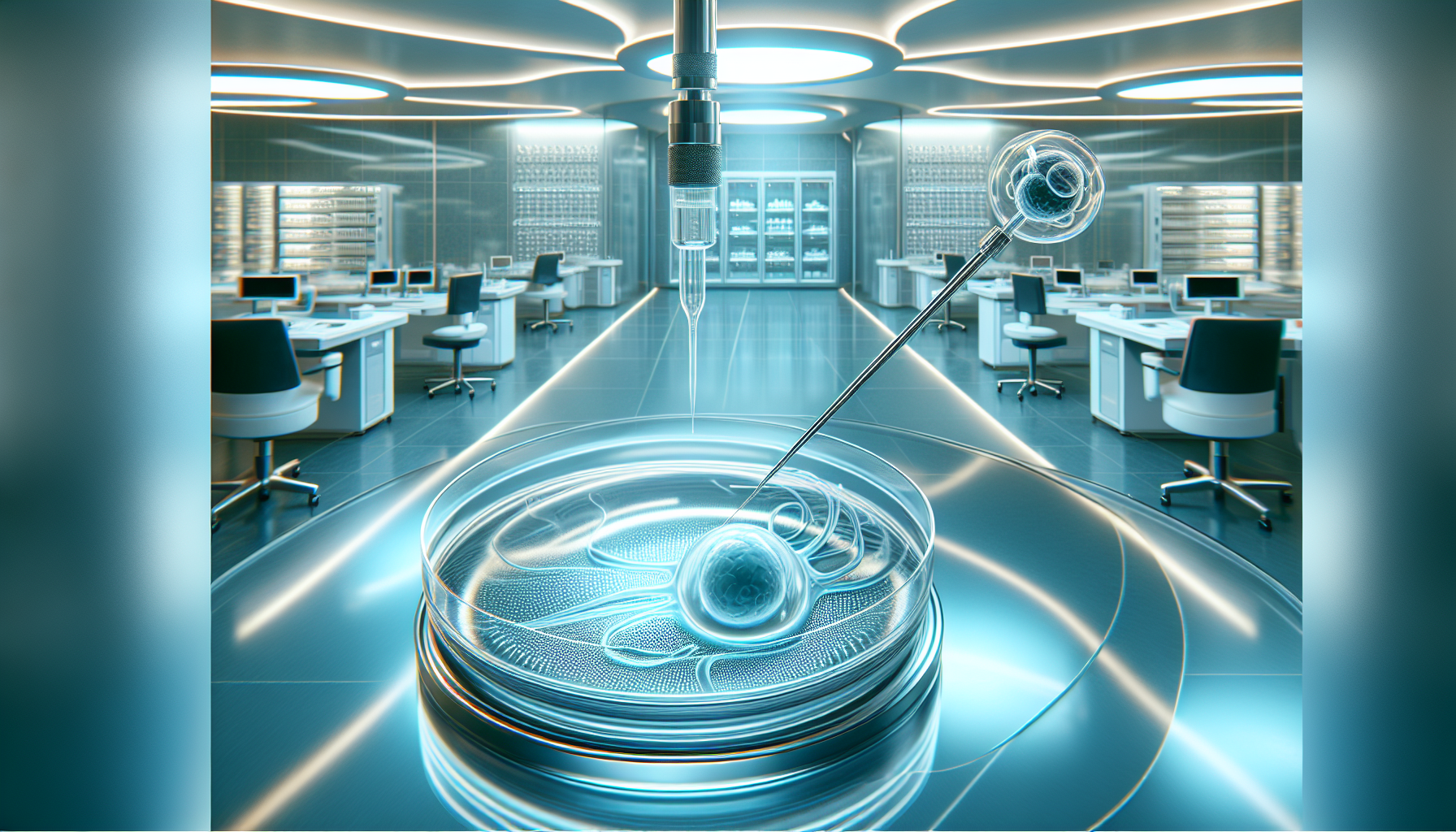
When post-thaw motility continues to remain low despite all efforts, fertility treatment options should be considered. In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI), in particular, can provide greater success rates for couples dealing with male infertility due to reduced sperm motility.
The complexity of IVF or ICSI may seem intimidating. These treatments are often a path to parenthood for many struggling with infertility issues. Through the process of egg fertilization using one single donated sperm via ICSI or eggs mixed directly with semen in a laboratory environment through IVF – couple’s hopes could become reality if successful!
In Vitro Fertilization (IVF)
IVF is a sophisticated sequence of steps in which an egg and sperm work together to achieve fertilization. The method has higher success rates than IUI does, but can also be more costly and invasive. A key component for reaching successful outcomes with IVF is the motility level of sperm. When total spermatic movement as well as progressive mobility are elevated, chances for effectiveness become much greater – and specifically through the use of Intra-Cytoplasmic Sperm Injection (ICSI), male infertility due to post thaw low motility may be addressed by incorporating fresh ejaculate samples or cryopreserved semen specimens from epididymal sources and even testicular ones into treatments.
Intracytoplasmic Sperm Injection (ICSI)
For couples suffering from male infertility because of decreased post-thaw sperm motility, ICSI may be a great alternative. It involves injecting one single sperm into an egg and can result in pregnancy rates comparable to traditional IVF. Success with this method varies, but it is known to produce fertilization levels ranging between 70% and 85%, as well as pregnancy outcomes standing at 24%-35%.
This highly targeted approach compares favourably with the accuracy of a precision guided missile, which makes ICSI potentially successful for managing fertility problems caused by low ejaculate motility or other factors related to infertility struggles among males.
Summary
We’ve journeyed through a complex landscape of fertility treatments, sperm motility, cryopreservation, and alternative treatment options. We’ve seen how crucial post-thaw motility is for successful IUI outcomes, the factors that can affect it, and strategies to improve it. We’ve explored the roles of semen analysis and quality control, as well as when to consider alternative fertility treatments like IVF and ICSI. Understanding these factors can empower you on your fertility journey, offering hope and a way forward.
Frequently Asked Questions
What is a good post thaw motility?
Sperm motility after thawing is normally estimated between 20% and 40%. The count may vary due to different ways of freezing as well as time period taken or counting chamber used when conducting the sample.
What is the post thaw motility of bull sperm?
The motility of bull sperm after thawing was recorded at 50%. Abnormalities were also noted in the cells. At thirty minutes post-thaw, an average of 52.7%+/- 6.9% was determined for its level of movement and 41.6%, observed as the best value, showed optimal mobility when following a certain protocol during the process.
Does freezing sperm reduce motility?
Sperm motility can be reduced to an extent after going through the freeze-thaw cycle, but it does not have a major effect on pregnancy rates. Although there might be a decline of around 50% in sperm mobility, this still doesn’t significantly affect the chances of getting pregnant.
How long does sperm live after thaw?
Research indicates that sperm which has been defrosted can remain viable inside the human body for up to three days after it is inseminated.
How much sperm is in each vial?
When it comes to fertility treatments, the amount of motile sperm in each vial can be extremely important. A range between 10.5 and 19.5 million total motile sperm exists for ICI vials while IUI vials hold somewhere between 7 and 13 million total motile sperm available per sample used during a treatment cycle. Knowing this information is key when administering either type of application using these two types of samples containing various amounts of male reproductive cells necessary for successful fertilization results!


