Having a baby is one goal that many couples aspire to achieve. Nothing compares to bringing new life to the world. Unfortunately, some people have problems with their fertility, making it difficult for them to have a baby.
In the past, this meant the end of the line for their dreams of raising a family. However, modern technology now gives couples multiple fertility options such as artificial insemination. Artificial insemination, which is one of the most popular methods and is relatively straightforward, effective, and safe. This technology was first developed to breed livestock but now adopted for use in humans.
What Is Artificial Insemination?
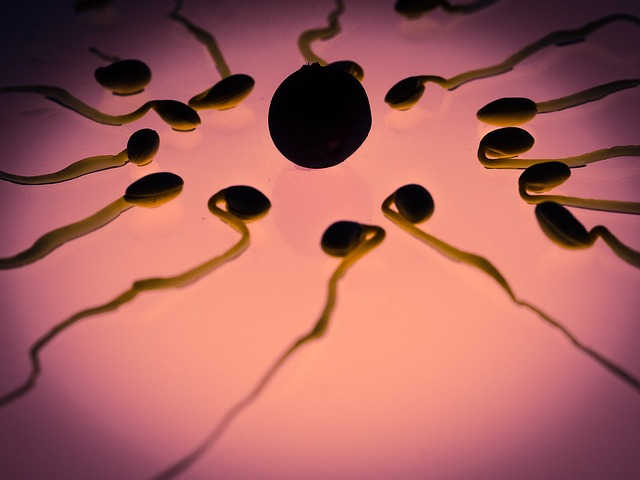
During sex, natural insemination occurs when a man ejaculates semen into his partner’s vagina. Sperm cells then travel upwards through the rest of the female reproductive tract until they reach and fertilize the egg cell.
Artificial insemination uses equipment to deposit sperm into the female reproductive tract, but the insemination site needs choosing so that the sperm have to travel less. This technique increases the chances of fertilization. According to Frances E. Shields, M.D., “Before inseminations are even planned, the physician should talk to both the husband and wife and be informed as fully as possible concerning their sincerity, their emotional stability, and their intellectual capacity.”
There are two types of artificial insemination, and the processes are depending on the site where they place the sperm cells. Intracervical insemination, or ICI, places the sperm cells on the cervix, while intrauterine insemination, or IUI, puts them in the uterus.

In Vitro Fertilization vs. Artificial Insemination
In vitro fertilization (IVF) and artificial insemination (AI) are both assisted reproductive technologies used to achieve pregnancy, but they differ significantly in their methods and applications:
Artificial Insemination (AI):
-
Process: Sperm is directly inserted into the woman’s cervix or uterus, bypassing the natural travel through the Fallopian tubes.
-
Indications: Used for conditions like male factor infertility, unexplained infertility, and single women or same-sex couples seeking pregnancy.
-
Success Rates: Success rates vary based on factors like female age, cause of infertility, and type of AI used.
-
Advantages: Less invasive and generally less expensive compared to IVF.
-
Disadvantages: May not be as successful as IVF for certain types of infertility.
In Vitro Fertilization (IVF):
-
Process: Involves egg retrieval, fertilization with sperm in a laboratory dish, and the subsequent transfer of the resulting embryos into the woman’s uterus.
-
Indications: Used for various infertility factors like severe male or female infertility, blocked Fallopian tubes, and some genetic conditions.
-
Success Rates: Generally higher success rates compared to AI, especially in cases of severe infertility.
-
Advantages: Offers a higher chance of pregnancy for certain types of infertility.
-
Disadvantages: More invasive, expensive, and time-consuming compared to AI.
Choosing between AI and IVF depends on the specific needs and circumstances of each individual or couple. Consulting with a fertility specialist is crucial to understand both options, their success rates, potential risks, and associated costs involved in making an informed decision that best suits their situation and goals.
What Conditions Can Artificial Insemination Be Used For?
Artificial insemination is useful for bypassing several fertility conditions that would otherwise impede fertilization. As an example, a couple that cannot perform sexual intercourse but otherwise produces healthy sperm and egg cells is a right candidate for artificial insemination.
For males, artificial insemination is useful for low sperm counts or low sperm motility, which is when the sperm cells are too weak to reach the egg cell by reasonable means. For females, artificial insemination is useful when the woman’s cervical mucus, which the sperm have to pass through, is too unfavorable for sperm survival.
Another condition that can warrant artificial insemination is endometriosis, which is when cells that form the inner lining of the uterus start growing elsewhere. This condition can lower fertility rates, but artificial insemination can be used to bypass any diseased areas.
Sometimes, a woman may be allergic to specific components of donor sperm.
In this case, artificial insemination allows the sperm to be processed to remove any allergens.
Subfertility caused by other factors, such as radiation treatment, can make it hard to conceive. Artificial insemination can offset the difficulty, which makes conception easier.
In general, artificial insemination suggests for couples who fail to conceive despite having one year of unprotected sex. If the woman is at the age of and above 35 years old, six months of no pregnancy can already be enough to warrant artificial insemination.
Artificial insemination is required if a couple wishes to use a sperm donor. This technique might be useful if the male has a genetic disorder that he does not want to pass on to his child. Same-sex couples can also conceive using artificial insemination using donated sperm.
What Should You Expect To Do For Artificial Insemination?
Timing is a crucial part of artificial insemination, as the depositing of sperm should as a woman ovulates. To do the procedure, there is an ovulation testing kit given to the woman, which can be used to predict when she will release an egg. She may also be asked to undergo regular ultrasounds and temperature measurements to confirm if she has ovulated or not. “AI may be performed following a natural ovulation or after inducing ovulation with ovary-stimulating medication,” Dr. Liji Thomas, MD says. In some cases, she might be asked to take medications, such as Clomid, to make her ovulate.
Once they set the ovulation date, there is another date set for sperm collection. If the sperm is to come from the male, he will usually be asked to avoid sexual activities for around two to five days before the collection day. This precaution ensures that sperm counts are sufficiently high once they did the collection. During the collection day itself, the male will be asked to collect semen with a sterile container. Due to the limited lifespan of sperm cells outside the body, the collection is preferably done in the clinic unless the couple lives up to an hour away from the facility.
Semen collection is commonly through masturbation or a collection condom used during sexual intercourse. If sexual activity is challenging, surgical sperm aspiration can be used to extract sperm cells directly from the male reproductive tract.
For ICI, they usually conduct the procedure in an office.
A doctor injects the collected semen into the vagina, near the cervix, using a special syringe. Aside from a needle, a cervical cap can be used to keep the sperm on the cervical opening for a set amount of time.
During this time, the woman is told to lie down for 15 to 30 minutes, allowing sperm sufficient time to travel to the uterus. After around two weeks, a pregnancy test is conducted to see if the procedure was successful.
For IUI, the same steps apply, but additional procedures are done to process the collected semen. The sperm cells are washed, removing some proteins and other components which might hinder successful fertilization. Washing also makes the sperm cells more concentrated. The sperm cells are then placed inside the uterus using a catheter. A speculum is used to keep the vagina open during this procedure.
Timing of Insemination
The timing of artificial insemination is crucial for maximizing the chances of pregnancy. It revolves around the woman’s menstrual cycle and identifying the fertile window, the period when ovulation takes place. This window typically occurs around 14 days after the first day of her last menstrual period.
There are two main approaches to determine the timing of insemination:
1. Static timing: This method involves performing insemination at a predetermined time within the woman’s cycle, often around the middle of the expected fertile window. This approach is simpler and more convenient but may not be as precise for all individuals.
2. Ovulation prediction: This approach involves identifying the specific day of ovulation using various methods, such as:
-
Ovulation predictor kits: These test urine for hormonal changes that indicate ovulation is approaching.
-
Basal body temperature (BBT) tracking: This involves taking daily morning temperature measurements to identify a slight rise that occurs after ovulation.
-
Ultrasound monitoring: This allows doctors to visualize the ovaries and follicles, providing a more accurate picture of ovulation timing.
By utilizing these methods, the doctor can determine the optimal timing for insemination, tailoring it to the specific characteristics of the woman’s cycle.
Estimated Cost and Insurance Coverage
The cost of artificial insemination can vary significantly depending on several factors:
-
Type of insemination: Intrauterine insemination (IUI) is generally less expensive than intracervical insemination (ICI).
-
Sperm source: Using donor sperm typically incurs additional fees compared to using a partner’s sperm.
-
Facility and doctor’s fees: Different clinics and doctors may have varying charges.
-
Number of insemination cycles: Each insemination attempt may involve additional costs.
While insurance coverage for artificial insemination varies across providers and plans, it’s becoming increasingly common for certain types of coverage. Some plans may cover specific aspects of the procedure, such as:
-
Diagnostic tests: Tests to determine the cause of infertility may be covered if deemed medically necessary.
-
Medications: Fertility medications used to stimulate ovulation might be partially covered depending on the plan.
-
Procedural costs: Some insurance plans may offer coverage for certain types of insemination procedures, especially when used for medically diagnosed infertility reasons.
It is vital to consult with your insurance provider to understand your specific plan’s coverage for artificial insemination. Be sure to ask about specific details such as:
-
Deductible: The amount you need to pay out of pocket before insurance starts covering the cost.
-
Co-pay: A fixed amount you pay for covered services.
-
Coinsurance: A percentage of the covered cost you share after meeting the deductible.
-
Lifetime maximums: The total amount your plan will cover for a specific condition throughout your lifetime.
Knowing your coverage details will help you budget for and make informed decisions regarding artificial insemination.
How Successful Is The Intrauterine Insemination?
The ICI procedure has a success rate of around 37.9% after six treatments. For the same number of treatments, the IUI procedure has a success rate of 40.5%. The higher success rate of IUI attributes to the additional preparation steps done on the sperm cells, as well as the placement of the cells nearer to the egg cell. Drew Moffitt, M.D., FACOG notes that “The success rate of artificial insemination does vary significantly with each patient, as different medications and transplanting techniques may be used in certain situations. The age of the female partner is also very important for the chances of success.”
Are There Any Side Effects to Artificial Insemination?
Some cramping and light bleeding can sometimes occur during the insemination procedure, but overall, the process is painless.
Infection is sporadic if the system conducted is in a professional clinical setting; it is still possible. The vagina serves to protect the rest of the female reproductive tract from infection, so bypassing it can lead to some risk.
If the woman is made to ovulate using Clomid or is taking other fertility medication, there is a significantly higher chance of having twins or triplets. It should be accounted for when planning for a family. A pregnancy with multiple fetuses has a higher risk.
Rarely, the medications used to stimulate ovulation can cause ovarian hyperstimulation syndrome or OHSS. The ovaries swell due to overstimulation, causing bloating and abdominal pain. Rarely, dehydration and shortness of breath can occur. Severe cases will need hospital admittance.
Are There Other Alternatives to Artificial Insemination?
If artificial insemination is insufficient, the couple may consider in vitro fertilization or IVF. This procedure involves extracting both sperm and egg cells from the couple. As the name implies, propagation is in the laboratory under controlled conditions. The most viable fertilized eggs implanted in the uterus of the female.
Doctors usually recommend artificial insemination for up to six cycles only. Additional treatments after this point are unlikely to yield results. At this point, people generally consider IVF.
If you already have a donor and would like to do it without the help of a clinic, you can use this home sperm test to check the fertility of your specimen. You can purchase the home sperm test here.
Frequently Asked Questions
How is artificial insemination done?
The sperm is inserted directly into the uterus, cervix or fallopian tubes. It cuts the travel of the sperm and it eliminates any obstruction. The most used method is intrauterine insemination.
How much does it cost to get inseminated?
Intrauterine insemination costs between $300-$1000 per cycle. If you opt for a sperm donor, per vial costs $700-$1000. On the other hand, intracervical insemination is around $200-$350 per cycle.
What is the difference between artificial insemination and IVF?
There is a clear difference between artificial insemination and IVF. IVF or In Vitro Fertilization involves stimulating the egg, retrieving, fertilizing, and transferring. Meanwhile, artificial insemination directly puts the sperm into the uterus to reduce the length and time of sperm travel.
What are the 4 types of artificial insemination?
The four different types of artificial insemination are:
Intracervical insemination is where the semen is placed in the cervix using a needless syringe. It is the easiest and most affordable.
Intrauterine insemination involves washed sperm introduced to the cervix using a catheter. It has the highest success rate because of its efficiency.
Intrauterine Tuboperitoneal Insemination is almost like intrauterine insemination except that the sperm is injected into the fallopian tubes. A clamp is placed in the cervix to prevent leakage.
Intratubal Insemination is where the sperm is injected in the fallopian tubes alone through a catheter.
How long is artificial insemination?
The procedure for artificial insemination is short which lasts around 15-45 minutes. It is relatively painless but cramping and bleeding are normal. Some say that the experience is like undergoing pap smear.
Can you get pregnant if you insert sperm with a syringe?
Yes, it is possible to get pregnant using sperm in the syringe. Semen must be injected into the vagina with a syringe during ovulation for a higher chance of getting pregnant.
What is the success rate of artificial insemination?
The success rate of intracervical insemination is around 10-15% per menstrual cycle. On the other hand, for intrauterine insemination, the success rate is 15-20% per menstrual cycle. After undergoing 6 cycles, there is a 60-70% chance of pregnancy.
Can you have twins with IUI?
There is an increased chance of having multiple pregnancies with IUI. If there are multiple eggs released in ovulation, the chances of fertilizing more than one egg increases.

Disclaimer: The information on this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images and information, contained on or available through this website is for general information purposes only. Please see a medical professional if you need help with depression, illness, or have any concerns whatsoever. WE DO NOT OFFER MEDICAL ADVICE, COURSE OF TREATMENT, DIAGNOSIS OR ANY OTHER OPINION on your conditions or treatment options. SERVICES OR PRODUCTS THAT YOU OBTAIN THROUGH THIS WEBSITE are for information purposes only and not offered as medical or psychological advice, guidance or treatment.
We also use some affiliate links in this blog to help support continuous production of wholesome parenting content such as this. 🙂 Feel free to use them to show your support.

